Inside: Do you have urinary retention after childbirth and are looking for hopeful stories? Here’s my postpartum urinary retention story with a positive outcome, along with what helped me get through it. From going home with a catheter to finally being able to pee again, one week after birth.
I laid down on the cold, hard hospital bathroom floor, doubled over clutching my side. I didn’t know how I was going to stand back up – the pain was that intense.
The nurse (Joanne was her name) came in with my husband trailing nervously behind her.
“Get up,” she said meanly firmly.
I still say she said it “meanly”, but to this day, my husband is on Joanne’s side 100%.
Finally, they got me up and back into the hospital bed. The midwives and OB/GYNs came in and felt my abdomen, sure that what they were feeling in midsection was the top of my uterus.
I writhed in pain, but the doctors were still confident that two days postpartum, I could be discharged.
Good old nurse Joanne was at least good for something. She stood up to the doctors for me, demanding, “Something’s not right. Can you please check her again?”
They begrudgingly obliged. As they felt my abdomen, they hit just the right spot smack in the middle, and I moaned in pain.
A look of horror came over the midwife’s face, and she said quietly, “I don’t think that’s the top of her uterus. I think that’s the top of her bladder.”
My bladder was so full it had completely displaced my uterus, which was now on the right side of my body.
I needed another catheter right away, or my bladder would explode.

How’d Your First VBAC Go? Well, I Couldn’t Pee After Birth, So There’s That
THIS POST PROBABLY CONTAINS AFFILIATE LINKS. AS AN AMAZON ASSOCIATE, I EARN FROM QUALIFYING PURCHASES. YOU CAN READ OUR FULL DISCLOSURE POLICY HERE.
Let’s back up. How exactly did I end up in this predicament?
Postpartum urinary retention isn’t exactly a run of the mill condition. I would imagine most pregnant women have never even heard of it. I certainly hadn’t until I couldn’t pee after birth.
I’ll try to keep this short.
My first birth was technically an emergency c-section. It wasn’t all “they rushed me to the ER because the baby was going to die if they didn’t get her out ASAP”, but it was relatively nerve-wracking for a first labor and delivery.
For my second birth, I was pretty sure that I wanted to try a VBAC. But I had a c-section scheduled just in case because that baby felt HUGE.
The painful varicose veins in my nether regions shouted BIG BABY, no matter what the ultrasound said.
Thankfully, labor started on its own three days late, but the day before my scheduled c-section. After 24 hours of labor with an epidural halfway through, I started pushing.
Well, three hours later, the midwife said I would need some kind of intervention if he didn’t come out in the next 10 minutes.
I interpreted that as, “You will need another c-section after three hours of pushing,” and pushed like I’d never pushed before.
(“Intervention” actually meant use a vacuum, but hey, the perceived threat of another c-section after all that pushing got the job done.)
That baby boy finally came out with his arm up around his neck, which is why he got stuck in the first place.
Did I mention the nurse almost dropped him because he was 10 pounds?
Turns out that arm up around his neck plus the 10 pounds plus three hours of pushing caused an almost fourth degree tear AND paralyzed the nerves that help your bladder communicate with your brain.
But it took a couple days for the hospital staff to figure that out…
Related: What You Really Need In Your Postpartum Care Kit (from a mom of 5)

You Can’t Pee? No Big Deal, They Said, Until…
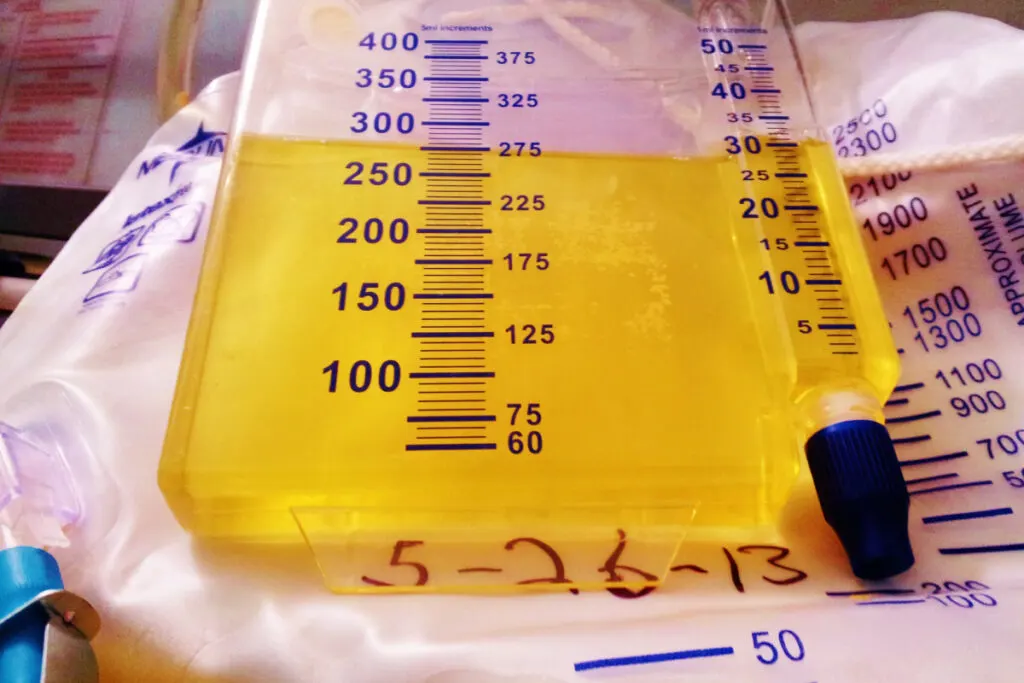
In the first 12 hours after birth, I was a mess. They give you that “hat” to pee in after birth to see if you’re peeing enough.
I wasn’t.
I couldn’t really push the pee out without risking breaking my fresh stitches. And doing anything hurt like a mother.
So after about 12 hours, they told me I should get a catheter back in, just for 24 hours to give my bladder time to recover.
No big deal, right? It was entirely depressing to need a catheter AGAIN, but the alternative was sitting on the toilet all the time, worrying whether I was urinating enough.
I agreed to give my bladder a break already.
After 24 hours, they removed the catheter again. And I was peeing…kind of.
I was going to toilet regularly, but not peeing a whole lot each time I went.
For some reason, they weren’t super worried about that. Or maybe they were just busy, I don’t know. Or maybe I didn’t speak up very much because I was afraid of needing another catheter.
Whatever the reasons, that’s how my bladder ended up extraordinarily full the morning I was supposed to be discharged. So full that it had pushed my uterus over and had me doubled over in pain.
That’s when they told me I had something called postpartum urinary retention (what the heck is that?!) and that I needed to go home with a catheter.
Talk about depressing.
What Exactly IS Postpartum Urinary Retention?
I’m gonna give you my down-to-earth definition. If you want the fancy medical one, see THIS article.
Essentially, I had pushed so long and so hard during labor that the pressure shocked my urinary nerves into not working anymore.
When you need to go, your bladder tells your brain, right? And when you sit on the toilet, your body is able to let the pee out, right? Normally, yes.
But when you have postpartum urinary retention, one or both of these two things happens:
- you no longer feel the urge to pee at all
- when you do feel the urge, you can’t let the pee out.
I struggled with the former for a few days. The “urge” finally came back, but then I struggled with the latter for months, but I figured out a work around that helped me to avoid long-term catheterization.
I’ll fill you in on that in a bit.

Going Home With a Catheter After Birth (Spoiler Alert: It Sucks)
So not only did I have a borderline fourth degree tear, I had to go home with a catheter.
We were also supposed to move in three weeks with a new newborn and a toddler. I’ve done it twice now, and the results are in: zero out of ten stars, do NOT recommend.
In short, I was an emotional a mess.
My grandfather had a catheter the last several years of his life, and now I realized why he always smelled like pee.
Catheters suck. No matter what you do, you always end up getting a little bit on you while emptying it.
Then factor in sleeping with it AND getting up in the middle of the night multiple times to feed a newborn with it.
YUCK.
A few days after first getting the catheter, I went in to the doctor to see if I could pee enough without the catheter. My mom was with me to watch the baby, thankfully.
I tried for an hour to pee more than a trickle – or at all! No luck.
With tears streaming down my cheeks, I had my fourth catheter of the week inserted to go home with. We scheduled an appointment for 3-4 days later.
Related: The Best Gifts for New Moms After Birth – What They Really Need

I Finally Did It! I Peed! (By Accident)
I showed up hopeful to my next appointment. I had to believe I was going to be able to pee.
The alternatives were a long-term catheter or learning how to self-cath. No thanks.
I got the catheter out, and the waiting game began.
I waited and waited and waited. I tried and tried and tried.
I had just about given up, when it hit me: I needed to poop.
I couldn’t pee, but hey, I figured I’d get my business done while I was catheter-free.
And guess what? All that pushing made the pee come out. Kind of. So I decided to push some more.
More pee came out.
I pushed that pee out like I was pushing a baby out (in moderation – I was still recovering). And out that pee came: enough to satisfy the midwives that I could go home without a catheter.
Finally.
Did I care that peeing was like labor for the next six months? Nope. I could finally feel when I needed to go pee again (thank you beautiful nerves!), and I was catheter-free, baby.
That’s all that mattered.

How to Cope If You Are Unable to Urinate After Birth
I will never forget the hopelessness I felt after realizing I couldn’t pee, and I would need a catheter after birth indefinitely.
I couldn’t even feel when I needed to go pee, for Pete’s sake!
Being able to pee is something we take for granted, right? Your bladder fills up; your brain tells you, and you go to the bathroom. End of story.
Well, no more. After having postpartum urinary retention, I am so freaking thankful every single time I urinate.
I remember feeling so depressed because I didn’t know when things were going to get better. When was I going to be able to be catheter-free?
If that’s you right now, here are my best tips on the other side of the whole experience.
Please Note: I am not a physician and am not in any way able to give medical advice. I am only sharing my own experiences with postpartum urinary retention and these should not be used to diagnose or treat yourself. All medical decisions should be made after consulting with a qualified OB/GYN or midwife.
1. Speak up right away if you are unable to urinate beyond a trickle in the span of 4-6 hours.
This was probably my key mistake. I could have let my body rest more and gotten the third catheter earlier.
But I was scared – scared of going home with a catheter and never peeing again.
I had done my googling, and I did not like what I found (see tip #2).
In retrospect, I should have spoken up. I could have had a catheter in another day and given my bladder more time to rest.
But I didn’t, and my bladder almost exploded.
My advice? Be honest. Save your bladder.
2. Whatever you do, DON’T read through forums with moms experiencing postpartum urinary retention.
You ended up here on this article. So, maybe too late?
I did a WHOLE lot of googling those first few days with a catheter. I read all the stories about women having ongoing problems for amounts of time I won’t mention here.
Don’t do it.
Stay positive: you’ll get through this.
Head to those forums if you’re still dealing with this two or three weeks after birth, and not before.
3. Invest in a pair or two of “catheter-friendly” pants that has buttons up the side.
These would have been so great to have when I had the catheter!
You really don’t want to be wearing shorts because then yuck, everyone and their mom can see the catheter strapped to your leg.
But pulling pants down and up and down and up to empty it is annoying and probably contributes to leaks (and therefore, smells).
Something like THIS pair, specifically designed for post-surgery or medical issues, would have be so amazing to have.

4. After a few days of bladder rest, try pushing the pee out.
This was the advice I didn’t get that would have helped me the most. I pushed pee out like I was pooping until about six months postpartum.
I discovered this by accident, and it’s the opposite of what doctors will tell you to do.
BUT IT BEATS GOING HOME WITH A CATHETER ANY DAY OF THE WEEK.
(Yes, that deserved to be bolded and all caps, thank you very much. If you know, you know.)
The doctors and nurses and midwives will tell you to “just let it come”. And I tried all the tricks they give you.
Pretend like you’re blowing bubbles.
Imagine the pee coming out of you.
Just relax.
Yeah, no. None of that worked for me. Pushing worked. Give it a whirl.
Just go easy if you have a lot of stitches, or wait a bit longer before you do.
5. Tell your postpartum urinary retention story when you can.
When you’ve recovered, and you’re peeing again? Tell your birth story – it deserves to be heard.
I had never heard of postpartum urinary retention! And every mom I talked to had no idea this could even happen.
Not being able to pee? Say what????!!
The ones who are going to read this post most likely have postpartum urinary retention. Or their partner does.
I don’t want to scare pregnant moms. But I do want women to be aware that this does happen, and women get through it.
If they know, they can bring it up with their providers and ask if they are at high risk of developing the condition after birth.
One study found an incidence of postpartum urinary retention around 5%. They noted in the conclusions of their study:
Postpartum urinary retention “was highly associated with epidural analgesia, forceps delivery, vulvar oedema, episiotomy, and second-degree perineal tears. More attention should be paid to women at high risk to reduce the incidence of PUR.”
Maybe telling your story could help someone?
There’s also something therapeutic about telling a birth story. I’m pretty sure it’s another thing that keeps the human race going: women processing intense and possibly scary labor and deliveries.

Birth Plans After Postpartum Urinary Retention
I went on to have three more babies after my second, postpartum urinary retention baby.
The fact that women forget the horrors of their birth experiences and go on to have more babies is a freaking miracle, I tell you!
For the next two births, my midwife and I made a plan to leave my catheter in for longer than usual.
Generally, epidural catheters are removed shortly after labor and delivery. In my case, they left it in for 8-9 hours after the third birth, and only a few hours after the fourth.
They were relatively easy labors. I guess 10 lb. baby #2 paved the way for his smaller siblings.
It might not be the best solution for you, or you might not even have an epidural where you have a catheter in the first place. But leaving the catheter gave me less anxiety, which is all I cared about.
If you plan to have more children, and especially if you change midwives, make sure to factor in a previous postpartum urinary retention experience into your subsequent birth plans.
Work with your midwive or OB/GYN to decide the best plan for you.
You Might Also Like: Retained Placenta Fragments: One Mom’s Scary Postpartum Experience

May You Pee Normally Again, Forevermore
I’ve been where you are. I wish I could give you a hug and have coffee with you, and tell you everything’s going to be o.k.
My blessing: may you be able to pee again every day, multiple times a day for the rest of your life. Without it feeling like labor.
Hold on to hope. Women get through this!
Women do go on to recover and pee normally again, catheter-free. Hang in there.
Read Next: What Does Postpartum Depression Feel Like? One Mom’s Story

Owner of Growing Serendipity, June could talk to you all day about homeschooling, parenting, and minimalism, which she does at This Simple Balance. When she’s not homeschooling, decluttering, or blogging, she loves to enjoy perfect silence while sipping a hot cup of coffee and thinking uninterrupted thoughts—which, of course, with five kids, doesn’t happen very often.